Are you at risk from impaired bone health?
Osteoporosis
The word ‘osteoporosis’ means ‘porous bone.’ It is a disease that weakens bones, and if you have it, you are at a greater risk for sudden and unexpected bone fractures. Osteoporosis means that you have less bone mass and strength. The disease often develops without any symptoms or pain, and it is usually not discovered until the weakened bones cause painful fractures. That is why Osteoporosis is called a “silent disease” because you may not notice any changes until a bone breaks. Most of these are fractures of the hip, wrist and spine.

After age 50, one in two women and one in four men will have an osteoporosis-related fracture in their lifetimes, with fractures of the proximal femur and vertebral body being associated with excess mortality over a 5-year period following fracture for both men and women.
Another 30% have low bone density that puts them at risk of developing osteoporosis. This condition is called osteopenia. osteopenia or low bone mass, consider it a warning. Bone loss has started, but you can still take action to keep your bones strong and maybe prevent osteoporosis later in life. That way you will be less likely to break a wrist, hip, or vertebrae (bone in your spine) when you are older.
Osteoporosis is responsible for more than two million fractures each year, and this number continues to grow. There are steps you can take to prevent osteoporosis from ever occurring. Treatments can also slow the rate of bone loss if you do have osteoporosis.
There is an estimated 20% mortality rate associated with a fragility fracture within the first year following the fracture and up to a 50% chance of sustaining a second fracture within the first 6 months following the sentinel fracture.
It is estimated that up to 40% of individuals who sustain a fragility fracture are unable to return to independent living and require nursing home care. And the lifetime risk of fractures will increase for all ethnic groups as people live longer.
The life-time risk for osteoporosis-related morbidity is greater than a woman’s combined risk for breast cancer, endometrial cancer, and ovarian cancer.
MEN AND OSTEOPOROSIS
THINK ONLY WOMEN ARE AT RISK OF OSTEOPOROSIS? THINK AGAIN.
The misconception is that men don’t get osteoporosis. The fact is that men frequently get osteoporosis and all too many of them are unknowingly suffering the consequences of this disease
Men are also more likely than women to require care in a long-term facility after a hip fracture.
Yet despite the fact that hip fractures can be more devastating for men than for women, men are less likely to be assessed for osteoporosis or to receive treatment for osteoporosis after they break a bone.
At least one in five men will break a bone from osteoporosis, and one quarter of the 30,000 hip fractures caused by osteoporosis in Canada are in men.
– In fact, every year approximately 7.500 Candian men will have a hip fracture from osteoporosis, which can be debilitating, and even life-threatening.
– While women are more likely to be assessed for osteoporosis after the age of 50.
– Both men and women over 50 should be assessed to determine their risk for fracture.
– The wrist, spine, shoulder and hip are common sites of Fragility Fractures from osteoporosis from a trip, slip or normal activity like coughing and sneezing.
What causes osteoporosis?
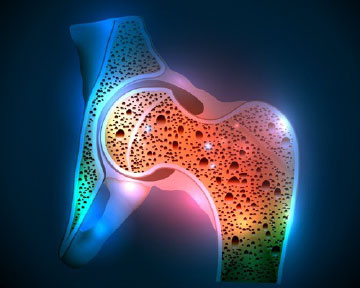
Researchers understand how osteoporosis develops even without knowing the exact cause of why it develops. Your bones are made of living, growing tissue. The inside of healthy bone looks like a sponge. This area is called trabecular bone. An outer shell of dense bone wraps around the spongy bone. This hard shell is called cortical bone.
When osteoporosis occurs, the “holes” in the “sponge” grow larger and more numerous, which weakens the inside of the bone. Bones support the body and protect vital organs. Bones also store calcium and other minerals. When the body needs calcium, it breaks down and rebuilds bone. This process, called bone remodeling, supplies the body with needed calcium while keeping the bones strong.
Up until about age 30, you normally build more bone than you lose. After age 35, bone breakdown occurs faster than bone buildup, which causes a gradual loss of bone mass. If you have osteoporosis, you lose bone mass at a greater rate. After menopause, the rate of bone breakdown occurs even more quickly.
Who is at risk for developing osteoporosis?
There are many risk factors that increase your chance of developing osteoporosis, with two of the most significant being gender and age.
Everyone’s risk for osteoporosis fractures increases with age.
However, women over the age of 50 or postmenopausal women have the greatest risk of developing osteoporosis. Women undergo rapid bone loss in the first 10 years after entering menopause, because menopause slows the production of estrogen, a hormone that protects against excessive bone loss.
Age and osteoporosis affect men also. You might be surprised to know that men over the age of 50 are more likely to have an osteoporosis-induced bone break than to get prostate cancer. About 80,000 men per year are expected to break a hip, and men are more likely than women to die in the year after a hip fracture.
Your risk of developing osteoporosis is also linked to ethnicity. Caucasian and Asian women are more likely to develop osteoporosis. However, African-American and Hispanic women are still at risk. In fact, African-American women are more likely than white women to die after a hip fracture.
Another factor is bone structure and body weight. Petite and thin people have a greater risk of developing osteoporosis because they have less bone to lose than people with more body weight and larger frames.
Family history also plays a part in osteoporosis risk. If your parents or grandparents have had any signs of osteoporosis, such as a fractured hip after a minor fall, you may have a greater risk of developing the disease.
Finally, some medical conditions and medications increase your risk. If you have or had any of the following conditions, some of which are related to irregular hormone levels, you and your healthcare provider might consider earlier screening for osteoporosis.
• Overactive thyroid, parathyroid, or adrenal glands.
• History of bariatric (weight loss) surgery or organ transplant.
• Hormone treatment for breast or prostate cancer or a history of missed periods.
• Celiac disease, or inflammatory bowel disease.
• Blood diseases such as multiple myeloma.
Some medications cause side effects that may damage bone and lead to osteoporosis. These include steroids, treatments for breast cancer, and medications for treating seizures. You should speak with your healthcare provider or pharmacist about the effect of your medications on bones.
• It may seem as though every risk factor is related to something that is out of your control, but that’s not true. You do have control over some of the risk factors for osteoporosis like:
• Eating habits: You are more likely to develop osteoporosis if your body doesn’t have enough calcium and vitamin D. Although eating disorders like bulimia or anorexia are risk factors, they can be treated.
• Lifestyle: People who lead sedentary (inactive) lifestyles have a higher risk of osteoporosis.
• Tobacco use: Smoking increases the risk of fractures.
• Alcohol use: Having two drinks a day (or more) increases the risk of osteoporosis.
Symptoms:
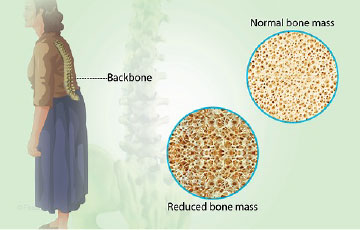
There typically are no symptoms in the early stages of bone loss. The first warning sign of Osteoporosis is Frequently a fracture But once your bones have been weakened by osteoporosis, you might have signs and symptoms that include:
– Back pain, caused by a fractured or collapsed vertebra.
– Loss of height over time.
– A stooped posture.
– A bone that breaks much more easily than expected.
Because the first warning sign of osteoporosis is frequently a fracture, it is often called “the silent thief” as it literally steals bone mass without giving any indication of doing so whatsoever, until a fracture occurs.
Complications:
Bone fractures, particularly in the spine or hip, are the most serious complications of osteoporosis. Hip fractures often are caused by a fall and can result in disability and even an increased risk of death within the first year after the injury.
In some cases, spinal fractures can occur even if you haven’t fallen. The bones that make up your spine (vertebrae) can weaken to the point of collapsing, which can result in back pain, lost height and a hunched forward posture.
How Can I Keep My Bones Strong?
Fortunately, osteoporosis can be prevented – with an early diagnosis before fractures occur, accurate assessment of bone mineral density, and early treatment. As in most implementations of preventative medicine, the “whole-person approach” usually results in the most successful outcomes. The backbone of a complete Bone Health Program, the whole-person approach requires…
• A lifestyle balance that includes appropriate nutrition and a strong understanding of the need for a healthy and balanced diet,
• An active lifestyle including regular exercises directed toward maintaining bone health,
• And appropriate bone health monitoring and medical treatment when necessary.
How can you prevent osteoporosis?
Your diet and lifestyle are two important risk factors you can control to prevent osteoporosis. Replacing lost estrogen with hormone therapy also provides a strong defense against osteoporosis in postmenopausal women.
Diet
To maintain strong, healthy bones, you need a diet rich in calcium throughout your life. One cup of skim or 1 percent fat milk contains 300 milligrams of calcium.
Besides dairy products, other good sources of calcium are salmon with bones, sardines, kale, broccoli, calcium-fortified juices and breads, dried figs, and calcium supplements. It is best to try to get the calcium from food and drink.
For those who need supplements, remember that the body can only absorb 500 mg of calcium at a time. You should take your calcium supplements in divided doses, since anything more than 500 mg will not be absorbed.
Recommended daily allowance of calcium
| Age and sex | Amount |
|---|---|
| Adults, 19-50 years | 1,000 mg |
| Adult men, 51-70 years | 1,000 mg |
| Adult women, 51-70 years | 1,200 mg |
| Adults, 71 years old and older | 1,200 mg |
| Pregnant and breastfeeding teens | 1,300 mg |
| Pregnant and breastfeeding adults | 1,000 mg |
Vitamin D is also important because it enables the body to absorb calcium. The recommended daily allowances of vitamin D are listed below. Vitamin D can also be obtained from sunlight exposure a few times a week or by drinking fortified milk.
Recommended daily allowance of Vitamin D
| People by age | Amount |
|---|---|
| Infants 0-6 Months | 400 IU |
| Infants 6-12 months | 400 IU |
| 1-3 years old | 600 IU |
| 4-8 years old | 600 IU |
| 9-70 years old | 800 IU |
| Over 70 years old | 800 IU |
| 14-50 years old, pregnant/lactating | 600 IU |
Talk with your healthcare provider about these numbers. In some cases, you might be told to take more vitamin D. Your provider might also have suggestions about the calcium type; for instance, you might be told to take calcium citrate instead of calcium carbonate. Calcium citrate does not need acid to work, so it may be a better choice for people who take antacids.
Lifestyle:
Maintaining a healthy lifestyle can reduce the degree of bone loss. Begin a regular exercise program. Exercises that make your muscles work against gravity (such as walking, jogging, aerobics, and weightlifting) are best for strengthening bones.
Do not drink too much alcohol. Do not have excessive amounts of caffeine. Don’t use tobacco at all.
What can you do if you are living with osteoporosis?
If you have osteoporosis, you should continue with the lifestyle measures mentioned earlier in terms of eating well, getting enough exercise, avoiding excessive caffeine and alcohol consumption, and not smoking. Make sure that you follow the suggestions of your healthcare provider. You should do all that you can to prevent falls inside and outside of your home. You might want to start with a medical evaluation, which could lead to your healthcare provider providing assistive devices.
Prevent falls inside your home
• Keep your floors free of clutter, including throw rugs and loose wires and cords. Use only non-skid items if you have mats, carpets or area rugs.
• Make sure your lighting is bright enough so that you can see well.
• Do not use cleaners that leave your floors slippery.
• Clean up any spills that happen immediately.
• Use grab bars in the bathroom and railings on stairways.
Prevent falls outside your home
• Make sure lighting is adequate in all areas outside your home.
• Use a backpack or other type of bag that leaves your hands free.
• Keep areas outside in good repair and free of clutter.
• Wear sensible shoes with non-slip bottoms.
This is in no way a complete list of things that you can do to help prevent falls, but this is a starting point. Also remember to take your time. You might be less careful if you are in a hurry.
When should you call the doctor about osteoporosis?
If you have risk factors and are concerned about osteoporosis, ask your healthcare provider about being screened, even if you are not as old as 65 (for women) or 70 (for men). Osteoporosis can be serious. Fractures can alter or threaten your life. A significant number of people have osteoporosis and have hip fractures die within one year of the fracture. Always call your healthcare provider if you fall, if you are worried about bone breaks, or if you have back pain that is severe that comes on suddenly.
Remember that you are able to lead an active and fulfilling life even if you do have osteoporosis. You and your healthcare provider can work together to make this happen.
When should osteoporosis be treated with medication?
Women whose bone density test shows T-scores of -2.5 or lower, such as -3.3 or -3.8, should begin therapy to reduce their risk of fracture. Many women need treatment if they have osteopenia, which is bone weakness that is not as severe as osteoporosis. Your doctor might use the World Health Organization fracture risk assessment tool, or FRAX, to see if you qualify for treatment based on your risk factors and bone density results. People who have had a typical osteoporosis fracture, such as that of the wrist, spine or hip, should also be treated (sometimes even if the bone density results are normal).
What medications are used to treat osteoporosis?
There are several classes of medications used to treat osteoporosis. Your healthcare provider will work with you to find the best fit. It’s not really possible to say there is one best medication to treat osteoporosis. The ‘best’ treatment is the one that is best for you.
– Hormone and hormone-related therapy:
This class includes estrogen, testosterone and the selective estrogen receptor modulator raloxifene (Evista®). Because of the potential for blood clots, certain cancers and heart disease, estrogen therapy is likely to be used in women who need to treat menopause symptoms and in younger women.
Testosterone might be prescribed to increase your bone density if you are a man with low levels of this hormone.
Raloxifene acts like estrogen with the bones. The drug is available in tablet form and is taken every day. In addition to treating osteoporosis, raloxifene might be used to reduce the risk of breast cancer in some women. For osteoporosis, raloxifene is generally used for five years.
Calcitonin-salmon (Fortical® and Miacalcin®) is a synthetic hormone. It reduces the chance of spine fractures, but not necessarily hip fractures or other types of breaks. It can be injected or it can be inhaled through the nose. Side effects include runny nose or nosebleed and headaches for the inhaled form. Side effects include rashes and flushing for the injected form. It is not recommended as a first choice. There are possible more serious side effects, including a weak link to cancer.
– Bisphosphonates:
Bisphosphonate osteoporosis treatments are considered antiresorptive drugs. They stop the body from re-absorbing bone tissue. There are several formulations with various dosing schemes (monthly, daily, weekly and even yearly) and different brands:
• Alendronate: Fosamax®, Fosamax Plus D®, Binosto®.
• Ibandronate: Boniva®.
• Risedronate: Actonel®, Atelvia®.
• Zoledronic acid: Reclast®.
You may be able to stop taking bisphosphonates after three to five years and still get benefits after you stop. Also, these drugs are available as generic drugs. Of these products, Boniva and Atelvia are recommended only for women, while the others can be used by both women and men.
Possible side effects of bisphosphonates include flu-like symptoms (fever, headache), heartburn, and impaired kidney function. There are potentially serious side effects also, such as the rare occurrence of jaw bone damage (osteonecrosis of the jaw) or atypical femur fractures (low trauma fractures of the thigh). The risk of these rare events increases with prolonged use of the medication (>5 years).
– Biologics:
Denosumab (Prolia®) is product that is available as an injection given every six months to women and men. It is often used when other treatments have failed. Denosumab can be used even in some cases of reduced kidney function. Its long-term effects are not yet known, but there are potentially serious side effects. These include possible problems with bones in the thigh or jaw and serious infection.
– Anabolic agents:
These products build bone in people who have osteoporosis. There are three of these products currently approved:
• Romososumab-aqqg (Evenity®) has been approved for postmenopausal women who are at a high risk of fracture. The product both enables new bone formation and decreases the breakdown of bone. You will get two injections, one right after the other, once per month. The time limit is one year of these injections.
• Teriparatide (Forteo®) and Abaloparatide (Tymlos®) are injectable drugs given daily for 2 years. They are parathyroid hormones, or products similar in many ways to the hormones.
Osteoporosis And Pregnancy:
Even though pregnancy induces certain health conditions, some of which can affect the mother badly, most of these health issues disappear after the delivery. However, sometimes, certain health conditions that induced in the course of pregnancy can be recognized only after the delivery. Pregnancy-induced osteoporosis is one among them.
What Is Pregnancy-Associated Osteoporosis?
Pregnancy related osteoporosis is an unusual condition that usually shows up (mostly) during the first pregnancy. The bones of the woman who experiences osteoporosis break easily during pregnancy or within a couple of weeks after delivery. The breaks usually happen in the spine, and sometimes in the hip. In spite of the fact that it can be painful and incapacitating for a period of time, the bones normally recover the break quickly and most women recover fully without affecting their day-to-day life. Pregnancy-associated osteoporosis is generally transitory, and as a rule, does not reoccur in the following pregnancies.
When Does Pregnancy-Associated Osteoporosis Affect an Expecting Mother?
Pregnancy-associated osteoporosis is mostly figured out during the postpartum period (56%) or during the third trimester (41%). It usually occurs during the first pregnancy and being temporary, once it goes away it does not happen again. The loss in bone density due to pregnancy and breastfeeding is temporary, and the full bone density can be recovered within 6 months usually.
What Causes Pregnancy-Induced Osteoporosis?
In pregnancy there is a noticeable passage of calcium from the mother to the baby that needs about 30 g of calcium, 80% only in the last quarter, with consequent lowering of the bone density of the pelvis and spine with a high-risk fracture also due to high weight gain and estrogen.
Also, some women are more prone to low bone density than others.
Maybe this will happen, when:
• Closely spaced pregnancies: Women who get pregnant before three months after the previous delivery may have a greater risk for osteoporosis than those who wait longer between babies
• Pre-existing condition: It is possible that some women already have low bone density before getting pregnant, either due to medications or due to the lifestyle
• Genetic factor: The researchers are not denying the role of the genetic factors when it comes to pregnancy related osteoporosis
• Increased bone metabolism: The bone metabolism increases during the third trimester, as the skeletal system of the baby is also developing and the bones are undergoing calcification. This will bring about extra withdrawal from the calcium bank thus adding stress to the mother’s skeleton
• Inadequate level of calcium and vitamin D: Inadequate calcium and vitamin D levels may result in the excessive ‘withdrawals’ from the calcium bank, bringing about the weakening of the bones in the course of pregnancy
• Heparin shots: Heparin injections taken prior to or in the course of pregnancy to treat a serious condition called anti-phospholipid syndrome, in some instances, result in pregnancy-associated osteoporosis
What Are the Symptoms of Pregnancy-Associated Osteoporosis?
There are no particular symptoms that indicate the issue of osteoporosis. However, the expecting mother experiencing osteoporosis often develops:
• Severe back pain
• Loss of height
• Vertebral fracture
How Is Pregnancy-Induced Osteoporosis Diagnosed?
Pregnancy-associated osteoporosis usually remains unidentified until the delivery. This is because there is no particular sign that specifies the condition of osteoporosis. Besides, back pain, the vital sign of osteoporosis, as the spine is more prone to its ill effects, is really common during pregnancy. Moreover, the procedures like bone scan and X-rays, which are used to diagnose the osteoporosis, is very dangerous to perform during pregnancy.
A fracture during pre-delivery or during delivery or during post-delivery generally leads to a diagnosis pregnancy-induced osteoporosis. As already mentioned, hip bones and ribs are more frequently susceptible to the fracture.
Echolight and pregnancy:
Now it is possible to evaluate the bone density of the vertebrae and the femur without the use of the X-rays through a simple radiation free technique (Echolight system using ultrasound) that will allow the clinicians to prescribe an appropriate therapy, increasing the intake of calcium and vitamin D if necessary to prevent the disease.
Echolight is only proved method to diagnose osteoporosis during pregnancy without any harm to the baby as it is using ultrasound.
Do the baby’s bones get affected due to pregnancy osteoporosis?
No, the pregnancy-induced osteoporosis has no harm effect on the bones of the baby. All the calcium deposition needs of the baby are full filled from the withdrawn calcium from the calcium bank of the mother.
What are the treatment plans for pregnancy-Induced osteoporosis?
• Fractures in vertebrae mostly heal on its own
• A fracture in the spine needs prolonged rest to heal
• Vitamin D and calcium supplements are prescribed to fix the bone density
• Medicines to get relief from the pain and that cause no harm during breastfeeding is prescribed by the doctor
• Hydrotherapy, the therapy is done in the swimming pool under the supervision of a physiotherapist, helps to relieve pain, as you feel weightless and easy to move around
• Transcutaneous Electrical Nerve Stimulation (TENS) machine is used in which, electrical impulses are utilized to block the pain signals
Can the mother feed her baby if she had pregnancy-induced osteoporosis?
Some doctors strongly disagree with feeding your baby if you have osteoporosis, as the breastfeeding will draw more calcium from the skeleton and can delay the recovery of your bone strength. However, breastfeeding is also a very personal, individual choice. If you insist you need to feed the baby, discuss the matter with the doctor. The doctor will try to find a solution to increasing the intake of vitamin and mineral supplement.
Oncology & Osteoporosis:
Osteoporosis can be caused by bone cancer or by certain types of cancer that spread to the bones. Cancer that has not metastasized (spread beyond its original site), increased inflammation both at the cancer site and throughout the body can lead to bone loss. The bones are also a common site of metastasis, affecting the skeleton.
Some forms of cancer treatment can also weaken bones, although they can improve survival. Cancer treatments may aim to reduce estrogen or testosterone to slow cancer growth (particularly when treating breast or prostate cancer). The blocking of these protective hormones can lead to bone weakening.
Cancer treatments that can increase the risk of osteoporosis include:
• Aromatase inhibitors, such as Femara (letrozole), Arimidex (anastrozole), Aromasin (exemestane)
• Gonadotropin-releasing hormone agonists, such as Zoladex (goserelin) and Lupron (leuprolide)
• Surgical removal of the ovaries or testes
• Androgen deprivation therapy, such as Casodex (bicalutamide), Eulexin (flutamide), Nilandron (nilutamide)
• Some people with brain tumours need to take antiseizure medicines (anticonvulsants) to prevent seizures.
• Steroids, such as prednisone and cortisone
• Some chemotherapy medications
• Medications that suppress the immune system, such as methotrexate
Types of cancer that may lead to bone loss include the following:
• Bone cancer
• Breast cancer
• Prostate cancer
• Lung cancer
• Multiple myeloma (cancer of the plasma cells)
In particular, those with bone and breast cancer are at increased risk.
When bone loss occurs due to cancer therapy, it can be more than seven times that of traditional aging. It is typically more rapid and severe.
Furthermore, Cancer treatment can exacerbate osteoporosis if this condition is already affecting patient bones.
Management of Osteoporosis With Cancer
Having either an increased risk for osteoporosis or osteoporosis outright can affect how your cancer is managed. Your oncologist (a doctor who specializes in treating cancer) will want to assess the chances that your bones will weaken and potentially develop fractures.
Some non-cancer-related risk factors they will weigh include the following:
• Your age
• If you are postmenopausal
• Whether you’re a cigarette smoker
• Whether you consume alcohol
• If you’ve had other fractures as an adult
• Whether your body is producing sufficient sex hormones
• If you are thin
• If your parents had a history of hip fractures
If you have a cancer diagnosis and have at least one other risk factor for osteoporosis, you will likely be asked to take a bone mineral density test. For cases in which your oncologist has prescribed an anti-cancer medication known to cause bone loss, this test should be repeated at least every one year, if not sooner.
You may be given bone-modifying medication to help lower the risk of fractures if you have osteoporosis or are at a high risk of developing it. These include bisphosphonates.
As a rule, hormone replacement therapies known to be protective of bone (such as estrogen replacement therapy), will be avoided if you have hormone-responsive cancer because it would stimulate cancer growth.
Prevention:
Having a diagnosis of cancer does not necessarily mean that you are destined to also develop osteoporosis. To help keep osteoporosis from occurring in conjunction with any cancer diagnosis, you will likely be advised to do the following:2
• Ramp up the amount of calcium and vitamin D that you consume. It will likely be recommended that you consume at least 1,000–1,200 milligrams per day of calcium and 800–1,000 international units (IU) per day of vitamin D.
• Quit smoking because it can affect bone quality and can otherwise heighten fracture risk.
• Give up drinking alcohol, which can affect your balance and otherwise lead to falls.
• Exercise to improve balance, strength, and flexibility and help reduce the chance of falls.
Echolight and cancer patients:
Echolight can help detect bone loss early, before it becomes a significant problem. Bone density measurements using echolight can provide accurate and reliable results that can guide treatment decisions. For example, if bone loss is detected, the patient’s doctor may recommend lifestyle changes, such as increased physical activity and dietary changes. In some cases, medication may be prescribed to prevent or manage osteoporosis.
Echolight can also be used to monitor bone density over time. Regular bone density measurements can help track changes in bone density and guide treatment decisions. This can be particularly important for cancer patients, who may undergo multiple rounds of treatment over the course of several years.
In addition to bone density measurements, echolight can also provide information on bone structure. This information can be used to identify fractures and other bone abnormalities, which can be particularly important for cancer patients who may be at an increased risk for bone fractures.
Overall, echolight can play an important role in the care of cancer patients by providing accurate and timely bone density measurements. By detecting bone loss early, patients can take proactive steps to prevent or manage osteoporosis, which can improve their overall health and quality of life.
Osteoporosis And Menopause
Menopause (the natural ending of periods that usually occurs between the ages of 45 and 55) can increase the risk of developing osteoporosis. The drop in estrogen levels that occurs around the time of menopause results in increased bone loss. Bone loss happens when the bones deteriorate faster than they can grow and strengthen themselves — and as much as 20% of bone loss occurs within your first five years of menopause.
How menopause influences osteoporosis?
Women reach peak bone mass around the age of 25 to 30 years, when the skeleton has stopped growing and bones are at their strongest and thickest.
The female hormone, estrogen, plays an important role in maintaining bone strength. estrogen levels drop around the time of menopause, which occurs on average at the age of 50 years, resulting in increased bone loss. If the peak bone mass before menopause is less than ideal, any bone loss that occurs around menopause may result in osteoporosis.
Research suggests that about one in two women over the age of 60 years will experience at least one fracture due to osteoporosis.
Is early menopause a risk factor for osteoporosis?
Menopause triggers bone loss, period. So, no matter when it happens to you, you’re at risk when it does. “Throughout menopause, women should be tested for osteoporosis,” Doctors advises.
But typical menopause happens between age 45 and 55, so if any women enter menopause before then, they’re also at risk for bone loss at an earlier age than is standard. That includes:
• Premature menopause (before age 40).
• Early menopause (before age 45).
• Primary ovarian insufficiency (POI), formerly called “primary ovarian failure.”
• Medical menopause, whether surgically induced or as a result of medical treatment, like chemotherapy.
How do you keep your bones healthy during menopause?
As soon as menopause makes its presence known, it’s time to talk to your doctor.
“It’s imperative to discuss and institute a bone loss prevention plan with your doctor when the first signs of menopause appear,” As a lot of doctors says. “It’s a great time to get a baseline bone density test and to go over your family history, lifestyle and medications, and what you can do to be strong and healthy.”
Reducing the risk of osteoporosis during menopause
Around the time of menopause, you can reduce your risk of developing osteoporosis by following a few lifestyle recommendations, such as:
• Aim for 1,300 mg of dietary calcium intake every day. This equals about three to four serves of dairy food. A wide range of non-dairy foods also contain calcium, such as calcium-fortified soy or almond drinks, firm tofu, almonds, brazil nuts, unhulled tahini, dark green leafy vegetables and fish with edible bones, such as sardines or tinned salmon.
• Do regular and appropriate weight-bearing physical activity, including resistance training exercise with weights (always do this type of exercise under supervision).
• Maintain adequate vitamin D levels. Vitamin D helps the body to absorb calcium. It is made in the skin following sun exposure, and is found in very small amounts in some foods. Vitamin D levels can be measured by a simple blood test.
• Avoid excessive alcohol intake (current guidelines recommend a maximum of two standard drinks per day with two alcohol-free days per week for women).
• Avoid smoking (smoking cigarettes is associated with a higher risk of developing osteoporosis).
• Avoid excessive caffeine intake.
These lifestyle habits are best started younger in life to get the most benefit.
Treatment:
Like mentioned above