BONE MINERAL DENSITY TEST
A BMD test can tell you whether or not you have osteoporosis

Why should I get tested?
Because osteoporosis and the correlated increased risk of fracture have devastating consequences, both for patient’s quality of life and for public health, resulting in heavy economic and social costs across the world . Therefore, an identification of patients at high risk of fracture is essential, and high sensitivity and specificity levels should be pursued in this field.
This is why medical testing is so important. The tests are known as Bone Mineral Density (BMD) tests and the technology that they use is known as bone densitometry. These tests are safe, painless and accurately measure the density of your bones. A BMD test can tell you whether or not you have osteoporosis and how likely you are to develop it in the future, and can help you to make decisions that may prevent fractures or further bone loss.
When used in combination with important clinical risk factors, a BMD test can help determine your fracture risk and assist your physician in making decisions about your treatment.
WHO SHOULD GET A BONE MINERAL DENSITY TEST?
- All women and men 65 years or older
- Postmenopausal women and men 50 – 64 with risk factors for fracture including:
- Fragility fracture after age 40
- Vertebral fracture or low bone mass identified on x-ray
- Parental hip fracture
- High alcohol intake
- Current smoking
- Low body weight, i.e. less than 132 lbs or 60 kg
- Weight loss since age 25 greater than 10%
- High risk medication use: prolonged glucocorticoid use, aromatase inhibitors for breast cancer, androgen deprivation therapy for prostate cancer
- Rheumatoid arthritis
- Other disorders that may contribute to bone loss
- Younger men or women (under 50) with a disease or condition associated with low bone mass or bone loss:
- Fragility fractures
- High-risk medication use (steroid use, aromatase inhibitors, androgen deprivation therapy)
- Rheumatoid arthritis
- Other chronic inflammatory conditions
- Cushing’s disease
- Malabsorption syndrome
- Uncontrolled hyperthyroidism
- Primary hyperparathyroidism
- Hypogonadism; Early menopause (< 45)
- Other disorders associated with rapid bone loss/fractures
- Pregnancy
- Diabetes
- Cancer treatment
- Family history of osteoporosis
BMD testing is not usually recommended in younger men or women (under age 50) unless there is a medical condition predisposing them to osteoporosis or when there are unexplained fragility fractures.
What To Expect During A Scan
There is no need to wear any special clothing; loose trousers and a top are fine.
You won’t need to completely undress, you simply expose two areas of your body (hip and tummy) when required.
The scan procedure is simple and painless. You are asked to lie on a couch fully dressed.
The first scan is of your hip so you will need to roll your trousers down to just above your knees. Some ultrasound gel is applied and you will feel a bit of pressure when the scan is in progress. This takes less than a minute.
The second scan is done on your spine through your navel area, so you will be asked to roll up your top for this. This scan is completed in under two minutes again with a little bit of gel and downward pressure.
The results are available immediately and are visible on the screen.
Your results are then emailed to you so you have them for future reference.
The whole appointment takes no more than 15 minutes.
But what exactly does EchoS tell you about your bone health?
Bone mineral density (BMO), This is an actual measurement of the density of the bone (measured in gr/cm2). The BMD is used to determine the T-Score and the Z-Score. A correct osteoporosis diagnosis is entirely dependent on accurate BMD data.
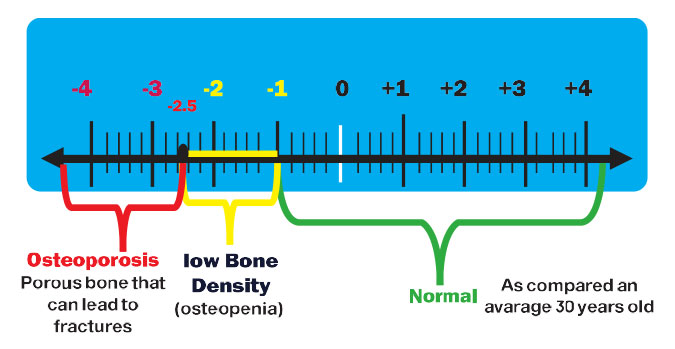
T-score, this is a numeric value derived through statistical calculations that directly compares an individual BMD to the mean BMD value of a very large database of healthy 30-year-old women. A T-score value with a standard deviation of -2.5 from the mean value establishes a diagnosis of osteoporosis.
Z-score, this is a numeric value derived in a similar manner as the t-Score, but instead, it compares your BMD to the BMD of people your own age and gender.
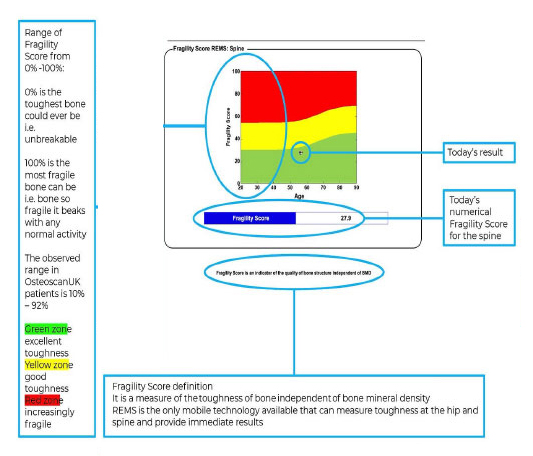
Fragility score, this is a numeric value derived through statistical calculations using data obtained during the EchoS Scan. After the data is compared to a database of people with and without fractures, the calculated value reflects the quality of your bone and how likely you are to sustain a fragility fracture.
So, What Echolight (The latest technology in osteoporosis detection) can help in?
1- Assess bone health without harmful ionizing radiation.
2- Produce an automated report within several minutes.
3- Determine precise and correct bone health data.
4- Analyse brand-new bone health information – the Fragility Score.
5- Help Clinicians give more accurate fracture risk assessments.
6- Allow for early detection and diagnosis of low bone density and osteoporosis.
7- Take a more proactive approach to bone health.
8- Predict fragility fractures for women and patients with type 2 diabetes or other risk factors.
9- Help in pre-operative bone assessment prior to joint replacement or spine fusion surgery.
Result of the scan
What is BONE DENSITY?
Currently, testing for bone density (or Bone Mineral Density — BMD) test has been the most common technique used to determine if someone has osteoporosis. BMD is the primary factor used in the DEXA (Dual-energy X-ray Absorptiometry) method.
The current understanding is that bones with a higher BMD are healthier and stronger and less likely to fracture.
However, bone density doesn’t provide a whole picture of bone health.
A denser bone is not always a stronger bone. For instance, sodium fluoride was once thought to be a suitable treatment for osteoporosis. Although fluoride effectively boosted measured bone density (BMD), it actually made bones more brittle and prone to fracture.
Bone health also can suffer without becoming excessively “thin.” Certain illnesses and medications can affect a bone’s structure without a measurable decrease in density, making the bone more likely to fracture.
In both of these circumstances, the bone quality was affected.

What is BONE QUALITY?
Although there is no precise, quantifiable definition of bone quality at this time, many medical professionals understand it as the combination of all bone properties that impact a bone’s resistance to fracture.
The concept of bone quality extends beyond BMD to include aspects such as bone microarchitecture, accumulated microscopic microarchitecture damage, collagen structure, mineral crystal size and composition.
BONE STRENGTH = BONE DENSITY + BONE QUALITY
Bone strength describes a bone’s resistance to fragility fractures. The stronger your bones, the less likely they are to break!
Although some professionals in the field of bone health consider BMD the best (if not the only) way to assess bone strength, research from the last few decades reveals that this is not entirely true.
That means DEXA technology, which only considers a bone density (BMD) measurement, has a limited ability to determine fracture risk.
Research shows that bone quality is important in determining a bone’s ability to keep from fracturing. Therefore, testing for bone quality is an important part of assessing someone’s bone health status and assessing the risk of sustaining a fracture.
To get a full picture of bone strength, it’s best to consult with a medical professional who uses technology, like the innovative Echolight EchoS technology, that can assess BMD as well as other aspects of bone quality.
~
Looking for accurate, complete bone strength testing? Go no further!
The BoneScan uses Echolight EchoS technology to provide comprehensive bone density AND quality testing and osteoporosis assessments.
Bone Mineral Density vs Bone Fragility:
Bone mineral density (BMD) refers to the amount of hard material contained
within a certain volume of bone. The hard material is primarily made-up of hydroxyapatite, a mineral compound composed of carbon, phosphorus, oxygen and hydrogen and collagen, a structural protein found widely in biological tissues. The organisation of hydroxyapatite and collagen can be in a very compact structure which is termed cortical bone or a much more honeycomb like structure which is called cancellous bone. The density of the two types of bone is quite different with the cortical bone being much denser than the cancellous bone. All of the bones in the skeleton have an outer rim of cortical bone and a variable amount of cancellous bone within. Understanding the density of bone provides little information about the likelihood of that bone fracturing because bone density does not describe how well made the bone is. This is particularly the case for the WHO diagnostic categories “normal” and “osteopenia”. There is a somewhat better correlation between bone mineral density and the risk of fractures in the elderly who have osteoporosis, but this may not hold true for younger, active women with low bone mineral density.
To fully characterize the behaviour of bone mechanically, its structure needs to be understood and this is only made possible by techniques that examine the degree of bone toughness in the spine and the hip. Toughness is the inverse of fragility – the lower the fragility the tougher the bone.
REMS measures the fragility of the hip and the four bones in the spine independently of bone mineral density. The ultrasound signals from the probe are analysed alongside those that are used to generate bone mineral density and two scores or provided with each REMS scan result within a few minutes. The BMD results can be compared to those that are generated by DEXA machines, but the Fragility Score (FS) is unique to REMS, which is the only technology available in the world that can provide real-time measurement of bone toughness at the hip and spine in a clinic setting.
Understanding the interaction between bone density and fragility is key to assessing bone health in a holistic fashion. A woman with a low body mass index, who is otherwise completely well and who has no other risk factors for impaired bone health, is likely to have low bone density. However, if she is very active and spends a considerable time putting a variety of different loads through her skeleton, she is likely to have tough bone. As a result, her risk of sustaining a fracture will below. The converse is also true and someone with a high BMI is likely to have a high bone density, but if they are not active their fragility might also be high and they may be more prone to fracturing. This is the situation that can be encountered in people who have type 2 diabetes. With advancing age and if people have conditions that predispose to both osteoporosis and fragility, decreased bone mineral density and increased fragility are to be expected and these women may sustain fractures as a result of very minor injuries. However, they do not make up the majority of women who have fragility fractures. These are women who have either osteopenia or normal bone on bone densitometry. For many years it was speculated that there was a problem with bone fragility but it could not be demonstrated routinely. Now, with the REMS fragility score module being available in the BoneScan, this conundrum has been solved and it is frequently the case that women with bone density not in the osteoporosis category have high fragility hence their predisposition to low energy fractures.
Understand Your Results:
Bone mineral density and quality results from EchoS are available immediately.
Two scans are done; one on your lower spine and the second on your left hip. If the left hip can’t be scanned (you might have had a hip replacement for instance) the right hip will be done.
– The results will show a number of scores/figures
– Bone mineral density is measured in g/cm2
– The report you will receive will show your BONE MINERAL DENSITY and also another graph to show your BONE QUALITY.
Bone Density:

Discordance:
“the discordance between sales and evidence should be a focus”
But what do we mean by this?
Osteoporosis is a systemic condition and, by definition, will be found throughout the whole skeleton.
A “discordant” bone density reading would be a score that is widely different between the hip and the spine (the two major weight-bearing areas of the body, and therefore the best indicators of OP). Any two readings that show a >1.0 standard deviation between hip and spine are called a “discordance” , unless there is a clear clinical reason for this difference (such as a being immobile for a length or time, or in a wheelchair etc).
Discordant scores (if no clinic evidence for them) strongly suggest that one of the scan ratings is incorrect and should be questioned; DEXA results often show these discrepancies. Many times this discordance is due to operator error or poor equipment calibration of the DEXA machines. A REMS scan has no operator error neither can it be incorrectly calibrated so discordances do not occur (again, unless there is a clear clinical reason). Therefore, if a woman has a DEXA scan showing a major discordance, and she has no obvious reasons for such a result, she should query the DEXA result with the local unit. If an answer is not forthcoming, asking for a second opinion is entirely reasonable and appropriate.
Concordance:
“the concordance between the teams’ research results”
A hip and spine T-score reading that fits the formula of having no more than 1.0 SD between the two scores, and is therefore a correct score.
SO WHAT DO ALL THESE NUMBERS MEAN?
Your bone densities are compared to those of a population of healthy 30-yr olds (this is the T-score).
A score of 0 means your bone density is equal to the norm for a healthy young adult. Differences between your bone density and this healthy young adult norm are measured in units called “standard deviations”.
The more standard deviations below 0, (indicated as negative numbers) the lower your bone density and the higher your risk of fracture.
A T-score greater than −1.0 is considered normal or healthy.
A T-score of between −1.0 and −2.5 indicates reduced bone density when compared to the average 30yr old. This is not osteoporosis but “OSTEOPENIA”, a transitional state between normal and osteoporosis.
A T-score of −2.5 or lower indicates that you have osteoporosis. The greater the negative number, the more severe the osteoporosis.
NB, if you are menopausal, the Z-score provides a more accurate picture than the T-score.
Your Results: Bone Quality (The Fragility Score):
The second page of your report will show you the FRAGILITY SCORE (FS) of your bones. This is an indicator of the QUALITY of your bone structure and is completely independent of your bone density readings.
Again the illustration is in the traffic-light format so easy to understand and interpret. You will receive one graph for your hip and another for your lumbar spine (as seen below).
The third page is your TOTAL RISK SCORE.
This is a combination of bone mineral density measured on the first page of your report with bone toughness as above (FS).
These two measurements give a composite estimate of likely fracture of the hip or spine in the next five years.
NB, the data on this page of the report has only been verified using the
Italian population.
Service Packages
Starter Package
- Two EchoS scans (spine and hip)
- Immediate results send to your email.
Mid-term follow up package
- 2 starter packages 4-6 months apart
Annual follow up package
- 3 starter packages during the same year
Maternity Package
- Starter package during any of our Fetoscan packages
CONTACT US:
We will get back to you as soon as possible.

